What is Brain Fog?

Struggling to concentrate or remember details? Brain fog could be clouding your clarity. From potential causes to what it really feels like living in a mental haze, we’re breaking down the science behind sluggish cognition, and serving tips for sharpening your circuitry.
As a 40-something working mom of two kids, I have what you might describe as a very “full” brain. Toss some perimenopause into the mix, and some days my memory seems to short-circuit (like when I suddenly forgot the debit card PIN I’ve had for years while getting gas). Other days, my mind feels like it’s spaced-out and hazy — like my head is literally in the clouds.
Sound familiar? If so, you might also be dealing with brain fog. While brain fog isn't a medical diagnosis, it can show up as trouble focusing, memory slips, or just feeling like you're moving in slow motion. For some, brain fog happens only once in a while, like the morning after one too many merlots. Others may feel like it happens on the daily.
Although anyone can have bouts of brain haze, women get foggy more frequently than men. That’s because we experience many of the conditions linked to brain fog more than men: hormonal changes during pregnancy and menopause, autoimmune diseases, and thyroid disorders, for example (sorry, ladies). [,2, 3]
So, what exactly is brain fog? Well, it’s different for everyone, says Hannah Holmes, Ph.D., a psychologist and a clinical assistant professor at Appalachian State University in North Carolina. It’s a collection of various cognitive-related symptoms that can include feeling like your brain is running in slo-mo, forgetting even familiar names and tasks, and having trouble focusing on chores, work, meetings—you name it.
The good news? It’s likely you can de-fog your noggin with some simple lifestyle tweaks. Here’s what you need to know.
What are the symptoms of brain fog?
What does brain fog feel like? The symptoms vary from person to person, says Saira Bhatti, M.D., a board-certified psychiatrist and psychotherapist based in New York City. But they could feel a little like this:
- It seems impossible to concentrate or stay focused at work, at home, wherever.
- You sometimes feel slightly confused or disoriented, like missing a turn when driving in a familiar place.
- You’re spacey and forget basic things, like turning on the dryer after loading it with wet laundry.
- Your brain just feels tired, like it needs to be plugged in somewhere to recharge.
- Your thinking seems to be crawling at half-speed.
- You make spur-of-moment decisions without really thinking about them—or can’t make a decision at all, like what to make for dinner.
- You have squirrel-brain and are easily distracted.
- You have trouble finding words (embarrassing example:recently I blanked for a second on the name of the “metal stabby thing” we use to spear food to put into our mouths).
- You lose your train of thought mid-sentence (wait, what was I saying?).
- You feel generally “out of it.”

The science of brain fog
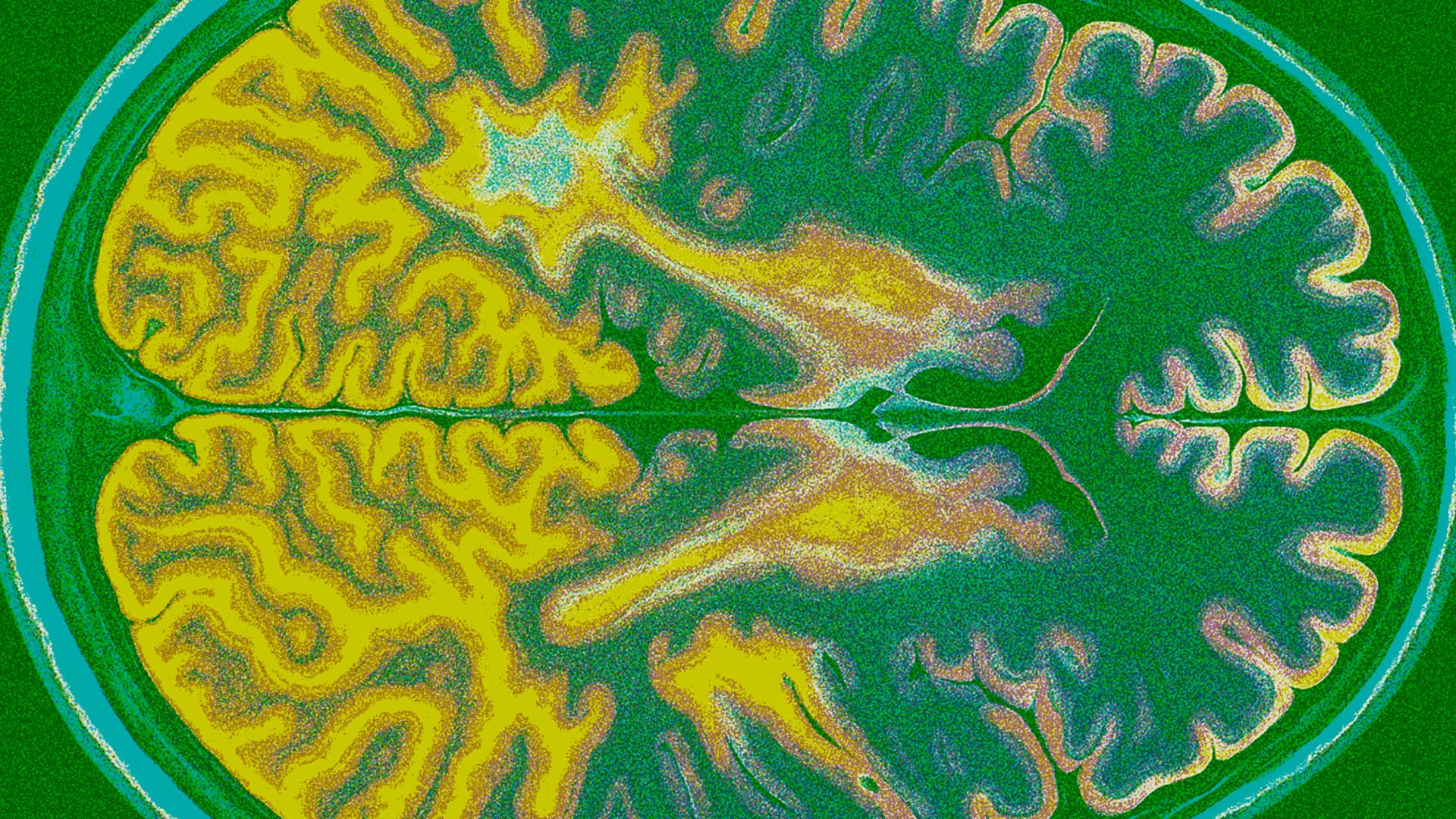
The exact step-by-step process of what happens in the brain when we get brain fog isn’t totally understood, in part because there are a number of factors that can cause brain fog. Plus, there’s no “standard” brain fog: It can look and feel different to everyone. But research has found a couple of strong correlations:.
Hormonal changes
In women, many times brain fog is tied to hormones, which is why it’s such a common experience when hormones go haywire, like during pregnancy and perimenopause. [4, 5]
Estrogen, in particular, plays a big role in cognition. The brain is full of estrogen receptors in areas that regulate mood and brain function. Estrogen has protective properties for the brain that can help shield the brain from damage and neurodegenerative diseases. It activates pathways in the brain to help brain cells grow and repair themselves. Estrogen also reduces inflammation and cell damage from oxidative stress. [6]
Inflammation
Inflammation may be a key driver of brain fog and can be caused by a number of factors. Research suggests that brain fog from long COVID may be linked to ongoing inflammation in the body and problems with the brain’s protective barrier, which can affect memory, learning, thinking, and mood. It’s thought inflammation is triggered by the immune system’s response to the COVID-19 virus. [7] Other research has also pointed to the link between cognitive impairment and inflammation in the tissue and organs (called peripheral inflammation). [8]
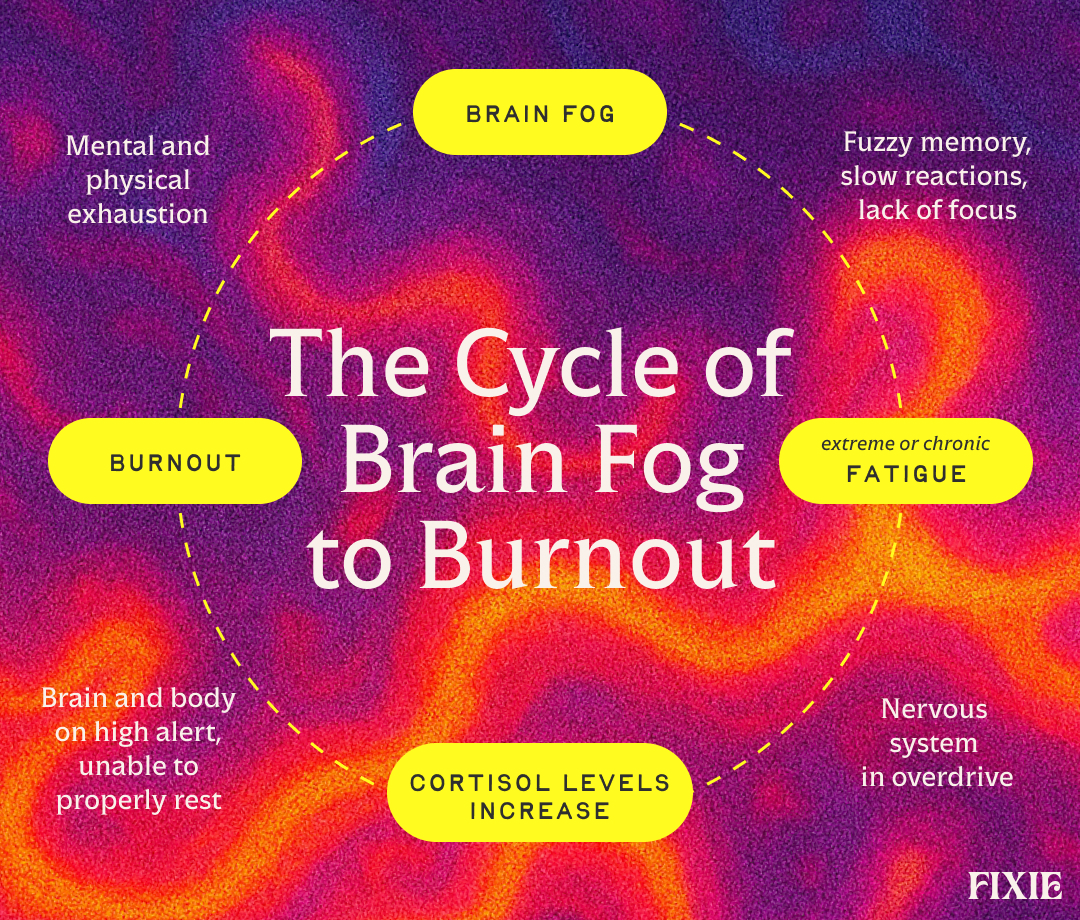
What’s the connection between brain fog and fatigue?
Brain fog and fatigue are “inextricably linked,” Holmes says. The brain and the body run on a feedback loop, with each informing and affecting the other. When our bodies feel wiped out, our brains feel zonked, too. The flip side of that is also true.
“When you feel physically exhausted, it is quite literally depleting the energy that your brain uses, too,” Holmes says. “So it makes sense that you would feel cognitively or mentally fatigued or foggy when you’re physically exhausted, and vice versa.”
When our bodies feel like they’re running on empty, our nervous system has to work harder to perform even pretty basic motor skills and mental activities. [9] When stress ramps up, so does cortisol — that stress hormone you’ve likely heard tons about on social media lately. Cortisol preps us for “fight or flight.” When stress is sky-high for long chunks of time, that cortisol keeps on pumping, holding our brains and bodies alert and tense. Try getting a decent night’s sleep when cortisol levels are high—not gonna happen. Eventually burnout hits, as neither the body nor the brain can sustain it.
“That burnout is often accompanied by depression or anxiety, which further fuels mental and physical exhaustion by disrupting sleep and serotonin levels,” Bhatti says. “It quickly becomes a cycle.”
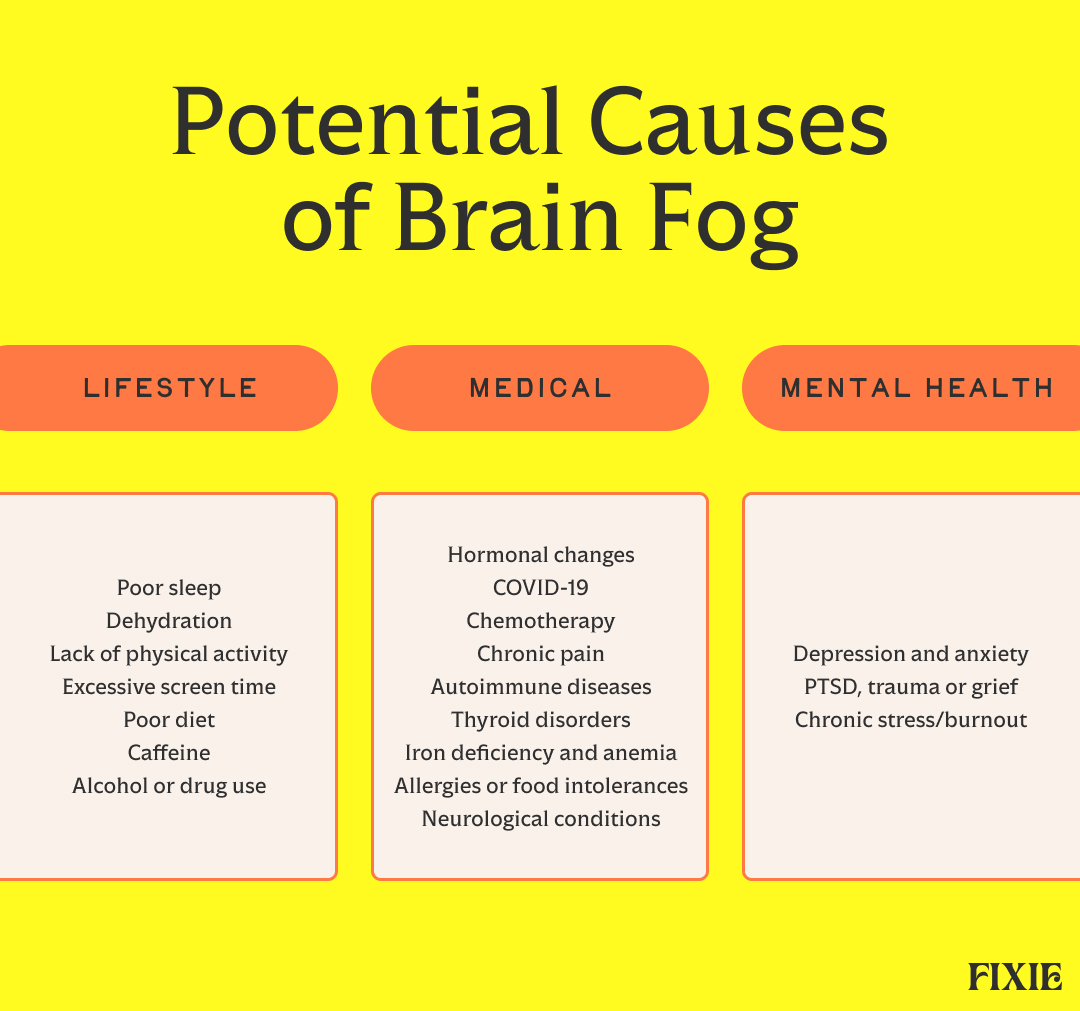
What causes brain fog?
Brain fog can pop up for all sorts of reasons — from not sleeping well, not drinking enough water, feeling stressed out, or dealing with chronic pain. In many cases, inflammation is the culprit, brought on by stress, diet, hormonal changes, health conditions, or other causes. [10]
Lifestyle causes of brain fog
- Poor sleep: This one’s a no-brainer. When we don’t get enough zzz’s, our bodies feel tired from head to toe. Research has found lack of quality sleep actually slows reaction time and impairs how well our brains work.[11]
- Dehydration: Time for more sips from that Stanley cup. Not drinking enough water can cause cortisol levels to rise. As a result, “feel-good” hormones like serotonin and dopamine plummet. Dehydration also causes an imbalance in our electrolytes, which further impacts cognitive function. [12, 13, 14, 15]
- Lack of physical activity: Need another reason to hit the gym? Your noggin needs exercise as much as the rest of your body does. In one study, too much sitting around was linked to worsening brain function – even in older adults who were otherwise highly active. [16]
- Excessive screen time: Yep, our phones are probably a problem. Marathon scrolling sessions or laptop time can strain the eyes, which makes our brains feel tired. Too much passive screen time (think: watching TikTok after TikTok after TikTok) may also lead to “digital dementia,” or increased forgetfulness. [17, 18]
- Alcohol or drug use: Alcohol and drugs directly damage the brain and can have long-term impact on memory, cognitive function, and executive reasoning. [19, 20]
Dietary causes of brain fog
- Added sugar: Consuming too much added sugar can have an impact on the brain as well as the body. Over time, sugar overload can fuel inflammation, which is thought to be a cause of brain fog. [21] The CDC recommends limiting added sugars to less than 10% of your daily calories (so, 200 calories or fewer of added sugar if you’re eating 2,000 calories a day).[22]
- Ultra-processed foods: Research has found eating overly processed foods was associated with an increased risk of cognitive impairment, while a diet composed of mainly unprocessed or minimally processed foods may lower that risk. What counts as an ultra-processed food? Many foods are processed (even frozen veggies), but ultra-processed foods tend to have lots of ingredients and additives (many of which could be found only in a lab). They’re often convenience foods that require minimal cooking or preparation. [23, 24]
- Caffeine: Ever tried to kick caffeine? Your head probably throbbed and felt like it was encased in mud. A little caffeine can make you feel alert and focused, but too much can have the opposite effect by trashing your sleep or making you feel scattered, anxious and jittery, Holmes says.
- Food allergies or intolerances: Research has found food allergies and sensitivities—like to gluten—can affect brain function and make you feel fuzzy. [25]
- Small intestine bacterial overgrowth (SIBO): SIBO is a condition in which too much bacteria grow in the small intestine, using nutrients needed for the rest of the body as fuel. In addition to gastrointestinal symptoms, SIBO can also cause brain fog. [26, 27]
- Iron deficiency and anemia: Anemia, including iron-deficiency anemia, commonly results in fatigue and brain fog. Iron deficiency and anemia affect women more commonly than men (thanks, menstrual periods). Iron is required to produce red blood cells, which shuttle oxygen to the brain. [28, 29]
- Other vitamin and mineral deficiencies: Nutrients like vitamin D, omega-3 fatty acids, vitamin B12, and magnesium help protect your brain from inflammation and oxidative stress. Not getting enough key vitamins and minerals in your diet can increase your chances of brain fog, cognitive decline, anxiety, and depression. [30, 31, 32, 33]
Medical conditions that can cause brain fog
- Hormonal changes: “The hormonal fluctuations women experience while pregnant and postpartum, combined with stress, fatigue, and sleep deprivation, create a perfect recipe for brain fog,” Bhatti says. “Similarly, hormonal changes that occur around menopause can contribute to brain fog.” [34]
- COVID-19: Cognitive problems, including brain fog and memory loss, are common symptoms associated with long COVID. So are fatigue, joint pain, and breathing issues. [35, 36]
- Cancer: Hair loss and nausea get a lot of attention when it comes to chemotherapy side effects, but brain fog is another one. [37]
- Chronic pain: Known as “fibro fog,” cognitive issues often accompany fibromyalgia and other similar conditions, Holmes says. [38]
- Autoimmune diseases: Many autoimmune disorders can cause brain fog, including multiple sclerosis (MS), lupus, and rheumatoid arthritis. And once again, women bear the brunt, as they account for nearly 80 percent of people with autoimmune disorders. [39, 2]
- Thyroid disorders: Both an overactive and underactive thyroid are commonly linked to issues with memory and concentration. [40]
- Diabetes: Both type 1 and type 2 diabetes can lead to brain fog, caused by imbalances in blood glucose and insulin. [41]
- Neurological conditions: Neurological diseases, including MS, dementia, and Parkinson’s, can cause brain fog. That’s due to inflammation and changes across the brain or central nervous system. Cognitive decline is the top symptom of dementia. [42]
Mental health conditions that can cause brain fog
- Depression and anxiety: Issues with memory and concentration are commonplace with depression and anxiety, potentially due to chemical or hormonal imbalances in the brain, poor sleep, and stress. [43, 39]
- PTSD, trauma or grief: Memory lapses, trouble with focus, and other cognitive issues are common symptoms of trauma or post-traumatic stress disorder (PTSD). The brain even interprets grief as a form of trauma. [44, 45]
- Chronic stress/burnout: Left untreated, long-term stress can wreak havoc on our bodies and brains. Stress is a major contributor to both burnout and brain fog, Holmes and Bhatti say.
- ADHD/Autism Spectrum Disorder (ASD): ADHD, ASD, and brain fog symptoms often overlap. Brain function and mental processing work differently in neurodivergent people, and memory, focus, and organization are common existing challenges. The mental fatigue and brain haze that commonly result from that persistent mental strain is often more long-term than in people who don’t have ADHD or ASD. [46, 47]
- Traumatic brain injury (TBI): Brain fog is commonly self-reported by people who are coping with a TBI, and it can be a significant obstacle in their recovery of memory and cognitive function. Research has found people with mild, moderate, or severe TBI have higher instances of brain fog than people who don’t have a TBI. In addition, brain fog was associated with higher rates of depressive symptoms. [48]
Only a healthcare provider can give you a clear diagnosis, but these scenarios might help you distinguish three memory-related conditions: brain fog, ADHD, and dementia. [49, 50, 51, 52]
- Johnson, H, et al. (2024) Journal of Health Psychology. Much more than a biological phenomenon: A qualitative study of women’s experiences of brain fog across their reproductive journey.
- Angum, F, et al. (2020). Cureus. The prevalence of autoimmune disorders in women: A narrative review.
- American Thyroid Association (n.d.) General information/press room.
- Barda, G, et al. (2021). Scientific Reports. The effect of pregnancy on maternal cognition.
- Peacock, K, et al. (2023). National Library of Medicine. Menopause.
- Guo, H, et al. (2020). Current Neuropharmacology. The critical period for neuroprotection by estrogen replacement therapy and the potential underlying mechanisms.
- Greene, C, et al. (2024). Nature Neuroscience. Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment.
- Tan, S, et al. (2023). Frontiers in Aging Neuroscience. Peripheral inflammation and neurocognitive impairment: correlations, underlying mechanisms, and therapeutic implications.
- Xu, R, et al. (2018) Frontiers in Neurology. How physical activities affect mental fatigue based on EEG energy, connectivity, and complexity.
- Geisinger (2024). What’s behind your brain fog?
- Khan, M, et al. (2023). Neurosciences. The consequences of sleep deprivation on cognitive performances.
- Zaplatosch, M, et al. (2020). Nutrients. The effect of acute hypohydration on indicators of glycemic regulation, appetite, metabolism and stress: A systematic review and meta-analysis.
- Dziurkowska, E, et al. (2021). Journal of Clinical Medicine. Cortisol as a biomarker of mental disorder severity.
- Dalvi-Garcia, F, et al. (2021). PLOS Computational Biology. A model of dopamine and serotonin-kynurenine metabolism in cortisolemia: Implications for depression.
- Sumitra, L K, et al. (2025). International Journal of Academic Medicine and Pharmacy. Hydration status and its impact on cognitive performance and reaction time in young adults: A comparative study.
- Gogniat, M, et al. (2025). Alzheimer’s & Dementia. Increased sedentary behavior is associated with neurodegeneration and worse cognition in older adults over a 7-year period despite high levels of physical activity
- Stanford Lifestyle Medicine (2024). What excessive screen time does to the adult brain.
- Moshel, M, et al. (2023). Neuropsychology Review. Neuropsychological deficits in disordered screen use behaviours: A systematic review and meta-analysis.
- National Institute on Alcohol Abuse and Alcoholism (2025). Neuroscience: The brain in addiction and recovery.
- Rezayof, A, et al. (2023). Neurochemistry International. Addictive drugs modify neurogenesis, synaptogenesis and synaptic plasticity to impair memory formation through neurotransmitter imbalances and signaling dysfunction.
- Gillespie, K et al. (2023). Nutrients. The impact of free and added sugars on cognitive function: A systematic review and meta-analysis.
- Centers for Disease Control and Prevention (2024). Get the facts: Added sugars.
- Bhave, V, et al. (2024). Neurology. Associations between ultra-processed food consumption and adverse brain health outcomes.
- American Heart Association (2020). Processed vs. ultra-processed food, and why it matters to your health.
- Zhou, L, et al. (2019). Behavioural Brain Research. Food allergy induces alteration in brain inflammatory status and cognitive impairments.
- National Library of Medicine (2024). Small bowel bacterial overgrowth.
- El Halabi, M, et al. (2024). Journal of Clinical Gastroenterology. Brain fog in gastrointestinal disorders: Small intestinal bacterial overgrowth, gastroparesis, irritable bowel syndrome.
- Munro, M, et al. (2023). American Journal of Obstetrics & Gynecology. The relationship between heavy menstrual bleeding, iron deficiency, and iron deficiency anemia.
- Gattas, B, et al. (2020). Cureus. The impact of low hemoglobin levels on cognitive brain function.
- Harvard Health (2022). Nutritional psychiatry: Your brain on food.
- Vellekkatt, F, et al. (2019). Journal of Postgraduate Medicine. Efficacy of vitamin D supplementation in major depression: A meta-analysis of randomized controlled trials.
- Dighiri, I, et al. (2022). Cureus. Effects of omega-3 polyunsaturated fatty acids on brain functions: A systematic review.
- Maier, J, et al. (2022). International Journal of Molecular Sciences. Magnesium and the brain: A focus on neuroinflammation and neurodegeneration.
- Barda, G, et al. (2021). Scientific Reports. The effect of pregnancy on maternal cognition.
- Denno, P, et al. (2025). Trends in Neurosciences. Defining brain fog across medical conditions.
- Fernández-de-las-Peñas, C, et al. (2023). Frontiers in Human Neuroscience. Trajectory of post-COVID brain fog, memory loss, and concentration loss in previously hospitalized COVID-19 survivors: the LONG-COVID-EXP multicenter study.
- Das, A, et al. (2020). Current Neuropharmacology. An overview on chemotherapy-induced cognitive impairment and potential role of antidepressants.
- Arthritis Foundation (n.d.) Fibro fog.
- Denno, P, et al. (2025). Trends in Neurosciences. Defining brain fog across medical conditions.
- American Thyroid Association (2022). Clinical Thyroidology for the Public. Hypothyroidism.
- Centers for Disease Control and Prevention (n.d.) Your brain and diabetes.
- Kouli, A, et al. (2024). Brain. Neuroinflammation is linked to dementia risk in Parkinson’s disease.
- Dobielska, M, et al. (2022). Frontiers in Psychiatry. Mechanisms of cognitive impairment in depression. May probiotics help?
- Békés, V, et al. (2023). Brain Research Bulletin. Competitive neurocognitive processes following bereavement.
- Dossi, G, et al. (2020). Frontiers in Psychiatry. Neural bases of cognitive impairments in post-traumatic stress disorders: A mini-review of functional magnetic resonance imaging findings.
- Attention Deficit Disorder Association (2024). Understanding ADHD brain fog: Causes, symptoms & treatment.
- Hale, T, et al. (2023). Neurology. Autistic burnout: A report of treatment success.
- Bell, T, et al. (2022). Research in Nursing & Health. Severity and correlates of brain fog in people with traumatic brain injury.
- University of Southern California Weill Institute for Neurosciences Memory and Aging Center (n.d.) Healthy aging.
- National Institute on Aging (2023). Memory problems, forgetfulness, and aging.
- Alzheimer’s Association (n.d.) 10 early signs and symptoms of Alzheimer’s and dementia.
- Attention Deficit Disorder Association (2024) 10 signs and symptoms of ADHD in adults (and when to get help).
- Nishi, S, et al. (2023). BMC Medicine. Water intake, hydration status and 2-year changes in cognitive performance: a prospective cohort study.
- Lin, M, et al. (2022). Activities, Adaptation, & Aging. Cognitive and socio-emotional benefits of puzzle working in older adults.
- Masuko, T, et al. (2024). Cureus. Efficacy of original neurofeedback treatment method for brain fog from COVID-19: A case report.
- Khasnavis, S, et al. (2024). Neurotrauma Reports. Combined use of guanfacine and N-acetylcysteine for the treatment of cognitive deficits after traumatic brain injury.
- Bowen, R, et al. (2023). Journal of Biophotonics. Use of either transcranial or whole-body photobiomodulation treatments improves COVID-19 brain fog.
- Felician, M, et al. (2023). Journal of Photochemistry and Photobiology. Photobiomodulation: Cellular, molecular, and clinical aspects.
- University of Southern California Weill Institute for Neurosciences Memory and Aging Center (n.d.) Determining a diagnosis.
Frequently Asked Questions
Brain fog is a decline in mental acuity that can manifest as forgetfulness, slower processing speeds, difficulty focusing, and cognitive difficulty.
It depends on the cause. If you regularly have trouble sleeping, are often stressed out, or don’t drink enough water, you may feel foggy more frequently.
It’s different for everyone, but it usually feels like your brain is working more slowly or sluggishly and you’re more forgetful or “spacey.” You may also feel forgetful and distracted.
That depends on what’s causing it. If it’s caused by a medical condition or medication you’re taking, it might not be easy to get rid of without the help of your doctor. But many easy lifestyle habits can help, such as adequate sleep, a well-balanced diet, stress-management practices, less screen time, and regular exercise. [11, 16, 17, 21, 30]
It depends. For some, brain fog can last a few hours. Others may find it lingers for weeks or even longer. It might pass relatively quickly if you’re hungover or didn’t sleep well, but it could last longer if it’s caused by a more chronic condition or a medication you’re taking. [1]
Brain fog and cognitive impairment have been linked to several vitamin and mineral deficiencies, including vitamin B-12, vitamin D, vitamin C, magnesium, iron, and omega-3 fatty acids.[28, 29, 30, 31, 32, 33]
Brain fog itself isn’t serious, but it can be a symptom or side effect of a more serious condition. Schedule an appointment with your healthcare provider to discuss your brain fog if you’re concerned or if it lingers and interferes with your work and personal life.
Latest Posts




.svg)