Perimenopause and Brain Fog: Causes, Symptoms, Relief

When hormones start to go haywire during perimenopause, your memory, focus, and mental energy are likely to take a hit. Not only that, but life probably feels like a three-ring circus of family, work, and other responsibilities most days. With this combo, it’s no wonder you’re feeling scattered. We get it—and we got you. Here’s what you need to know about perimenopause and brain fog, plus some tips for fixing it.
Here’s a weird flex: I’ve gotten extremely good at list-making over the past couple of years. I’ve always been a big proponent of writing down my to-do’s. But lately? Writing things down has become more of a must. It prevents my to-do list from becoming an “oh crap, I forgot” list.
As my 40-something self trudges toward menopause and away from menstruation, a scattered brain has emerged as one of my top symptoms of perimenopause so far. It’s not just a mental thing, though. How well I sleep, how much I exercise, what I eat, and how stressed I am all play a role in how smoothly (or not) my brain seems to operate. Some days I feel mostly normal. Other days I’d really like to speak to the manager about getting a refund because nothing seems to be working properly.
I know I’m not alone in this. Brain fog can happen to anyone for lots of reasons, but the hormonal shifts of perimenopause hit particularly hard when it comes to cognition. In fact, some estimates say 44% to 62% of perimenopausal women experience memory problems or other mild cognitive decline.
Sound like you, too? Let’s get to the bottom of perimenopause and brain fog, and explore simple habits and techniques for reclaiming our mental clarity.
Perimenopause and brain fog: What it is
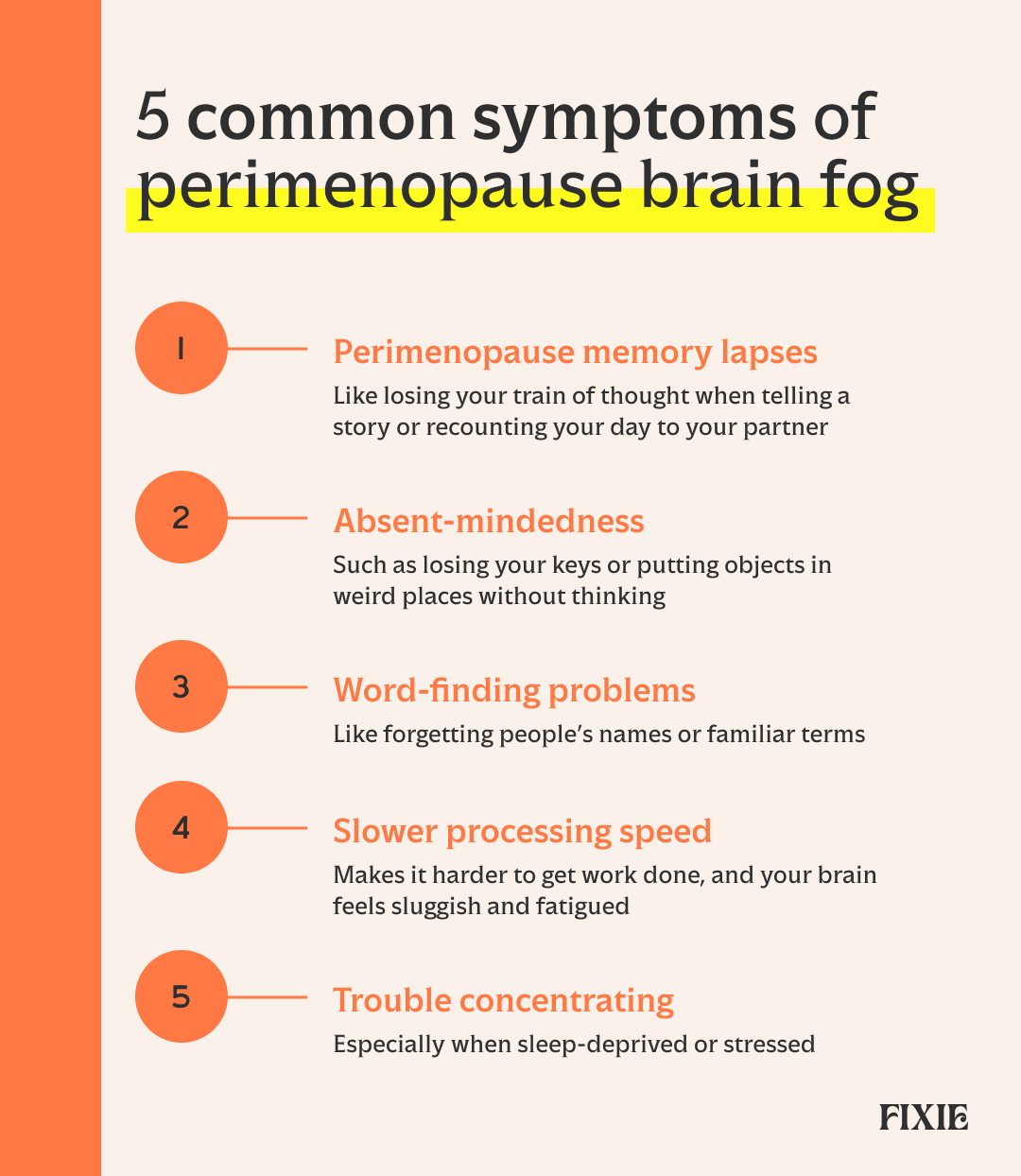
If your brain seems to be working at half-speed, if words are constantly on the tip of your tongue, or if you’re walking into rooms and forgetting what on earth you’re supposed to be doing there, welcome to the club.
Trouble with memory, learning, attention, and processing speed are all common occurrences for women in perimenopause. And even though perimenopause forgetfulness can be frustrating and even embarrassing (Aubrey’s mom with the blonde hair DOES have a name, I think…), most of the time these brain blips are not cause for alarm.
During this time, it makes sense to seek care from a practitioner who’s experienced in menopause and women’s hormonal health. A foggy brain is just one of many potential symptoms during this transition. Having a provider in your corner can be a big help, as you may need a plan or treatment for symptom management, either now or in the future.
Still, there are some simple habits you can put into place on your own that may help you breathe a little easier and think a little clearer. Let’s dive in.
Does perimenopause cause brain fog?
The short answer? Yes. But how?
To back up a bit: Menopause is really a moment in time, and it’s diagnosed retroactively, because it’s defined as 12 months without a menstrual period. Everything after that is postmenopause, and the timeframe leading up to that point is called perimenopause.
Perimenopause can last a long time—many years, in fact. The peri period usually starts in the late 40s to early 50s, though some women can experience it as early as their mid-30s. And here’s the kicker: perimenopause typically lasts five to 10 years.
During perimenopause, both estrogen and progesterone production start to decline. This hormonal decline has a wide-ranging impact on virtually every nook and cranny of the body, from our brains all the way down to the joints in our toes (women even experience completely bizarre symptoms like itchy ears and “frozen shoulder”).
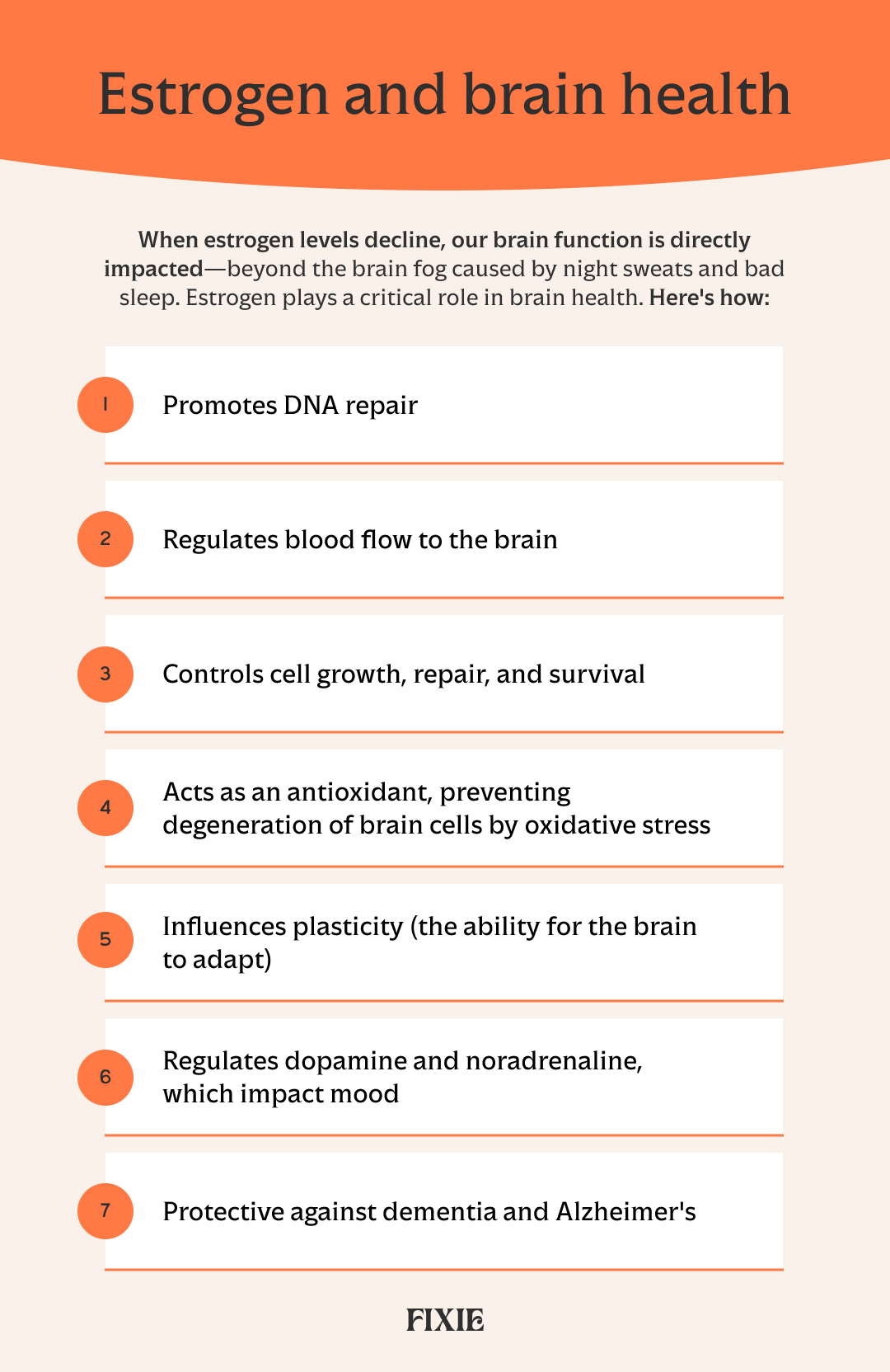
Fluctuating estrogen levels can influence attention, memory, and processing speed. It’s no wonder, as there are estrogen receptors all over the brain. Plus, estrogen has a regulating effect on the neurotransmitters serotonin and noradrenaline, so it’s not unusual for your mood to nosedive during this time, too.
Other factors that can lead to brain fog are poor sleep, high stress, and dysregulated mental health. During perimenopause, all of these symptoms are often intertwined, with one or more affecting others.
Let’s take a common menopausal experience as one example: night sweats. Imagine waking up in the middle of the night drenched in sweat. If it’s bad enough, you may have to get up and change your pajamas or even your bedding. A good night’s sleep? Not happening.
Now think about that fragmented sleep occurring a few times a week (or more). You’ll be both physically and mentally exhausted while you’re awake. You’ll be more stressed. You may even be anxious about going to bed because you’ll worry about waking up. And so the cycle continues. It’s no wonder we struggle to focus or remember people’s names.
But that’s not all. Estrogen has antioxidant and anti-inflammatory properties, regulates blood flow to the brain, and promotes DNA repair, among other neuroprotective benefits. So when estrogen levels decline, our brain function is directly impacted—beyond just night sweats and bad sleep.
For many women, perimenopause and its myriad of symptoms could not come at a worse time. We may be hitting the peak of our careers, only to feel sidelined by terrible sleep and issues with memory and focus. As “sandwich” adults, we might be trying to support our aging parents while still shuttling our kids to soccer practice. Talk about stress.
“Chronic stress has a strong connection to midlife cognitive symptoms, as it directly impacts memory and concentration through cortisol and other stress hormones,” says Brianna Paruolo, LCMHC, a licensed clinical mental health counselor at On Par Therapy in New York City, who works mostly with high-achieving women.
“During perimenopause, adrenal glands become the main source of hormone production, so chronic stress double-impacts cognitive functioning. Stress in combination with hormonal changes and poor sleep creates a perfect storm for brain fog.”

How common is perimenopause brain fog?
Feeling foggy and forgetful as you approach The Big M is very common. Research says 44% to 62% of women experience cognitive-specific symptoms of perimenopause, and up to 70% of women experiencing psychogenic symptoms. These are symptoms stemming from psychological causes, like stress or mental health conditions, rather than physical ones and may include anger or irritability, anxiety, depression, loss of concentration, and loss of confidence.
Every woman is different, though, and goes through this transition differently. Some have lots of symptoms, while others skate through pretty easily. Some may have hot flashes, and other women won’t. It’s all up to the “luck” of the draw.
How long does brain fog in perimenopause last?
For most women, symptoms ease once they move into menopause and hormones start to level out. Either way, the memory mishaps and hazy brain won’t last forever, nor does it mean you’re hurtling headfirst into dementia.
“It’s important to remember these temporary cognitive changes are related to hormonal fluctuation, not neurodegenerative disease,” Paruolo says.
Here’s a quick reference chart to determine if your symptoms need more attention.
Frequently Asked Questions
Perimenopause is different for everyone. What works for one person might not work for another, so it’s important to talk with a clinician about what’s at the root of your brain fog. Several treatment options are available, including hormone replacement therapy, lifestyle changes, and non-hormonal treatments.
Not everyone experiences brain fog the same way, but it can often look like forgetting people’s names, misplacing items like keys, inability to concentrate on work or other tasks, or feeling mentally tired or generally spacey and out of it.
Declining levels of estrogen and progesterone trigger a cascade of different mental and physical symptoms—many of which overlap. Night sweats can disrupt sleep, which can make you feel foggy, for example. Estrogen also directly protects the brain and affects neurotransmitter action, so when it declines, brain function may also decline.
No. In most people, brain fog related to perimenopause will resolve when hormone levels become more stable.
Foods rich in omega-3 fatty acids, B vitamins, iron, and other vitamins and minerals can support brain health. These include fatty fish, leafy greens, whole grains, berries, nuts, and seeds.
A multivitamin can fill in gaps in nutrition. If you suspect you may be deficient in certain nutrients, your healthcare provider can do bloodwork to check and then recommend other supplementation.
Yes. HRT can improve some menopausal symptoms, but it isn’t guaranteed to knock out all of them. If you still have brain fog while on HRT, ask your healthcare provider about other options that may help.
Latest Posts




.svg)

.jpg)
